Technology
Jackie had to change jobs over thoughts she might kill someone. New research shows why
From the outside, Jackie Morgan appeared to be an untroubled young woman with a bright future as a health professional ahead of her.
But internally, the Newcastle nutritionist was fighting off hellish thoughts of a fatal mistake on the horizon — she was convinced she was going to accidentally kill one of her clients.
WATCH THE VIDEO ABOVE:
Watch the latest news and stream for free on 7plus >>
“People who know me would actually have no idea I have OCD, because it’s completely internalised. You could be sitting opposite me and I would be going through OCD compulsions, and no one would know,” Morgan told 7NEWS.com.au.
The 28-year-old was only diagnosed with Obsessive Compulsive Disorder (OCD) four years ago, and said that until she started treatment last year: “I really hadn’t started living”.
It had reached such a point that Morgan quit her job, still fearful, paranoid, and unsure where her intrusive thoughts were coming from.
Now, groundbreaking research has confirmed exactly where the disorder originates in the brain.
OCD affects at least two per cent of the nation. That’s an estimated half-a-million Australians, many of whom can feel isolated by their experience.
“I gave up being a nutritionist, maybe six years ago. I was experiencing at the time what is known as harm OCD,” Morgan said.
“I was extremely paranoid that I was going to do or say or recommend something that was going to result in a client’s harm, and that could be something like recommending supplements, and they’re actually allergic (to it) and I didn’t know.
“It makes no sense, and it’s often very disconnected from reality ... but it just became so anxiety-inducing that I couldn’t do that job anymore,” said Morgan, who is now the OCD advocate behind You Me and OCD.
‘Magical thinking’
There are many different sub-types or “themes” with OCD, and Morgan said she has “pretty much experienced a majority of them”.
“When I was younger I had experienced more physical themes and compulsions, I had what’s called ‘magical thinking OCD’ which is where you think that if you think something it will happen.
Compulsions for magical thinking are often rituals or actions that the person experiencing the OCD will do to prevent that harm from happening, and prompt short-term relief from the distress caused by these thoughts.
“I would worry that if I didn’t do a specific set of rituals before bed ... something terrible would happen in the world, and that would have been my fault because I didn’t complete those rituals,” Morgan said.
“For example, I’d have to turn the tap off and go back to my bed three times, I’d have to wipe my hands along the back of the door three times, I’d have to lift up and lower my mattress three times, I had to pray three times, there was a specific prayer that I made up.
Just some of the many other sub-types include false memory OCD which creates doubt in the validity of real memories, and postpartum OCD which develops after giving birth and creates a fear of causing purposeful or accidental harm to the baby, according to the OCD Clinic Brisbane.
For many OCD sufferers the thoughts are disturbing and perverse.
QIMR Berghofer associate professor Luca Cocchi, one of the lead researchers behind groundbreaking OCD findings published this month, told 7NEWS.com.au these thoughts lead people to believe they are a bad person.
“When you have these horrible thoughts about killing someone or hurting people that are dear to you, you cannot stop the sense that you are a bad person.
“The reality is that, like for cancer and like for somatic things, these thoughts are all emerging from the brain, and there is a brain pathology.
“There is still this weird perception that what we think, what we are, is somehow dissociated from the brain. But if you have a stroke, if you have a tumour, your personality changes, who you are actually changes.”
Cocchi and Morgan Both believe the new research will be key to removing the stigma surrounding OCD and its symptoms.
Getting diagnosed
Morgan never knew she had OCD, she didn’t even know what it was — she had believed the persistent stereotype chalking up the disorder to a neurotic love of cleaning.
This minimised understanding of the disorder for Morgan was concurrent with what she said was: “The worst experience of OCD I had had, I was in a particularly dark place.”
She remembers the moment she stumbled across advocate Rose Cartwright’s description about OCD being characterised by intrusive thoughts, Morgan said: “I stopped in my tracks.” Cartright’s account drove Morgan towards her own life-changing diagnosis.
“Everyone is familiar with such intrusions. But not everyone is rendered intensely anxious by them, or feels compelled to spend hours every day trying to resolve, escape or explain them, Cartright wrote in a 2019 op-ed in The Guardian.
“The misconception of OCD is one of the major reasons it takes so long to be diagnosed, because we have no idea what it actually is.
“Having lived with OCD I know it’s nothing trivial or nothing enjoyable. It’s horrendous and horrific.”
Accessing treatment for OCD was a life-changing move for Morgan.
“The person I was a year ago, compared to today, are just totally different people,” she said.
Groundbreaking new research
The new QIMR Berghofer study published in the scientific journal Brain this month has ultimately confirmed the hypothesis that OCD is linked to a communication imbalance in the brain.
The breakdown in communication takes place between specific regions, within signalling pathways that are generally involved in key behaviour processing, including reward and emotion regulation.
“The regions are located in the front of our brain,” Cocchi, a lead researcher on the study, told 7NEWS.com.au. “We were basically able to define the pattern of communication between those regions.”
“One specific pathway is overactive, and one specific pathway is underactive.”
With this understanding, Cocchi said: “We can develop intervention where we excite or inhibit a given region so that you can really restore the communication.”
This type of targeted treatment does not currently exist. Medication similar to anti-depression medication, and cognitive behavioural therapy (CBT) are the two main treatments used to treat OCD, often used in conjunction.
But medication is an untargeted approach which affects the brain globally, and relies on metabolic factors among others. “So maybe some people will not respond to that,” Cocchi said.
“Behaviour therapy (also) doesn’t work for everyone. The behavioural therapy (for OCD) generally consists of exposing people to the source of their fear (ERP).
“Now, for example, if (a patient) has a fear of harming someone, they might be shown a picture of a knife or given a knife and so on, but this is very distressing and some people cannot tolerate that.”
While current treatments are not available to, or successful for everybody, the new findings — and potential for targeted brain stimulation treatments — is likely to lead to a huge expansion of accessibility.
-

 Technology11h ago
Technology11h agoHow We Picked the Best Inventions of 2024
-

 Technology17h ago
Technology17h agoTurning Simple Dresses into Statement Looks with Accessories
-
 Technology1d ago
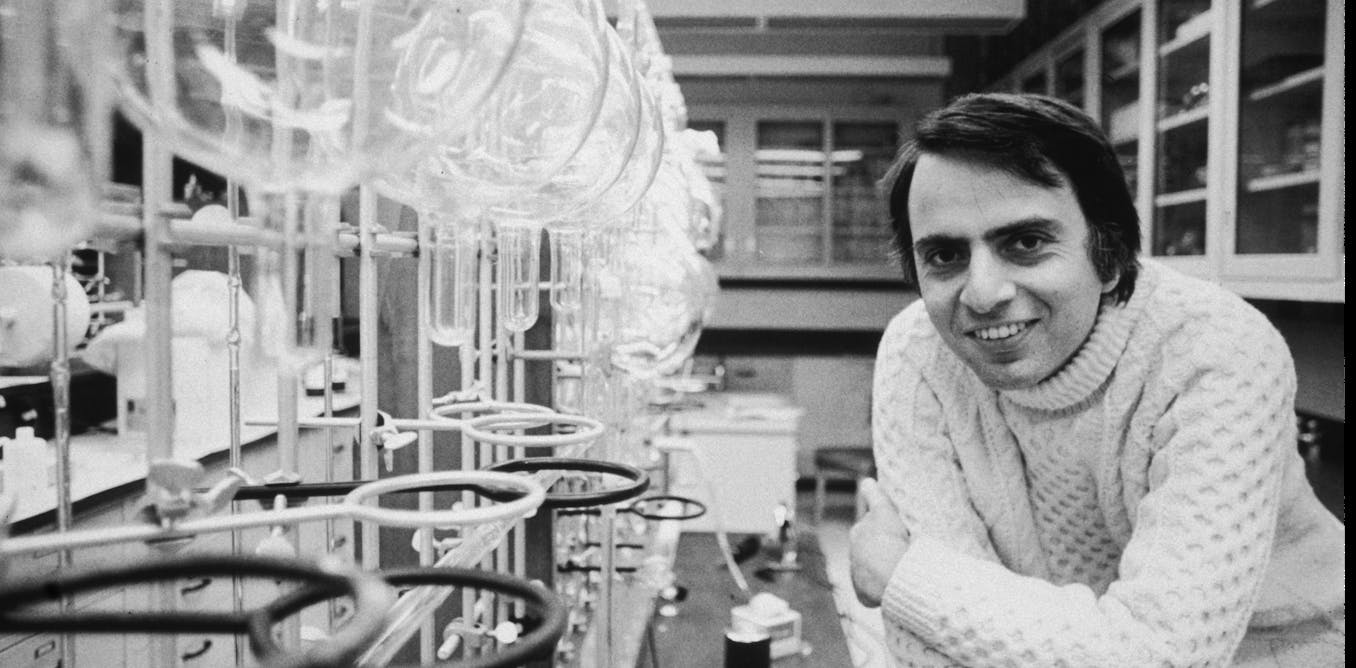
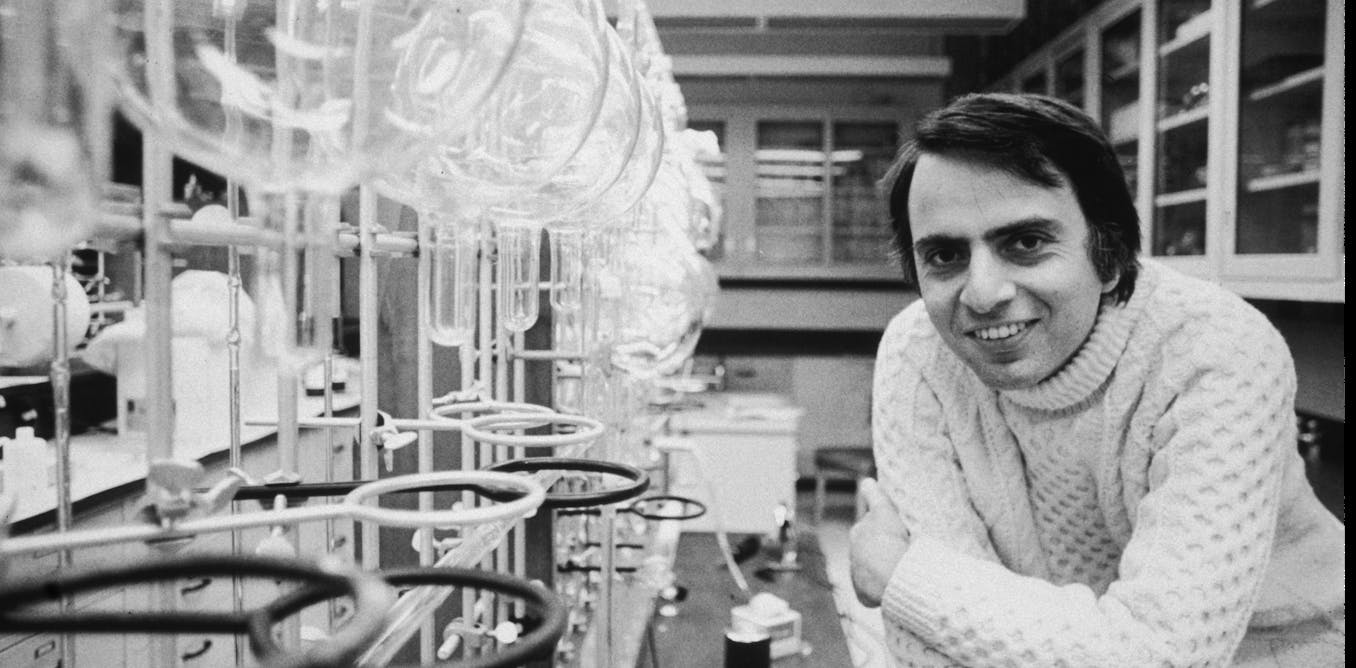
Technology1d agoCarl Sagan’s scientific legacy extends far beyond ‘Cosmos’
-
 Technology1d ago
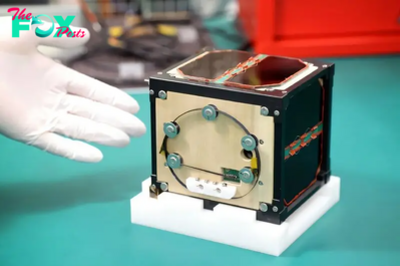
Technology1d agoJapan’s wooden satellite makes historic journey aboard SpaceX rocket to ISS | The Express Tribune
-

 Technology1d ago
Technology1d agoA Robot for Lash Extensions
-

 Technology1d ago
Technology1d agoThe 27 Club isn’t true, but it is real − a sociologist explains why myths endure and how they shape reality
-
 Technology1d ago
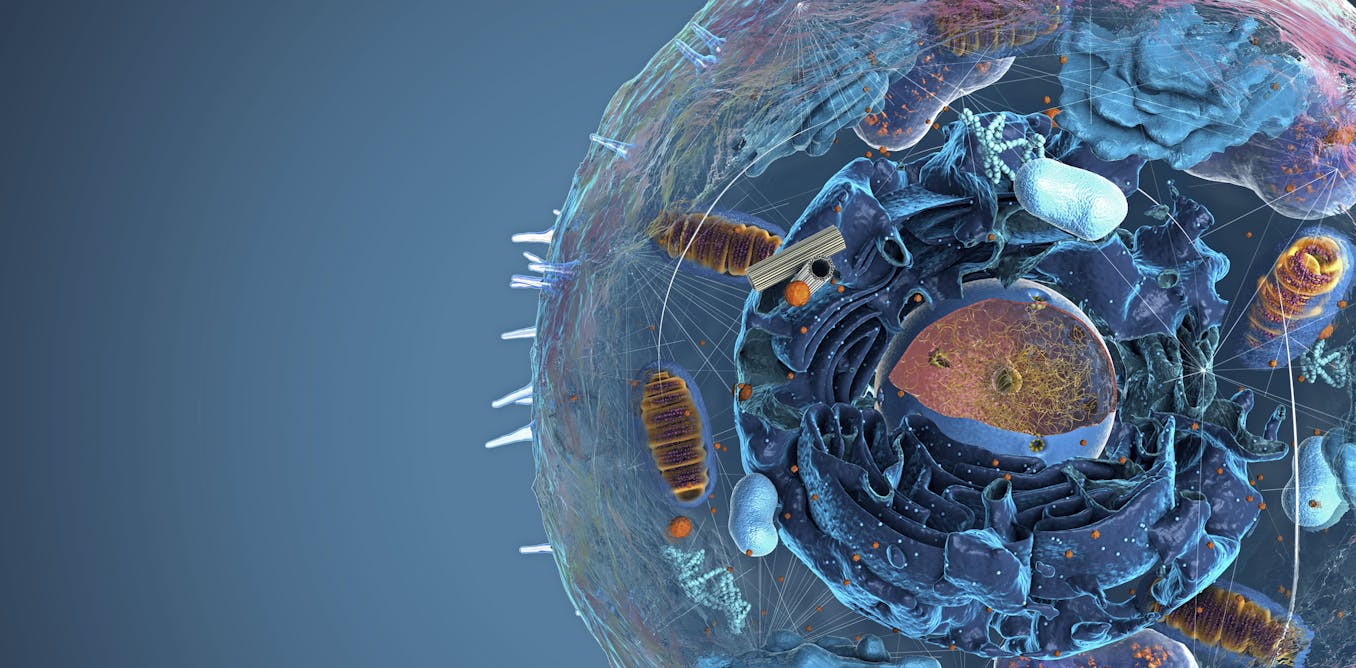
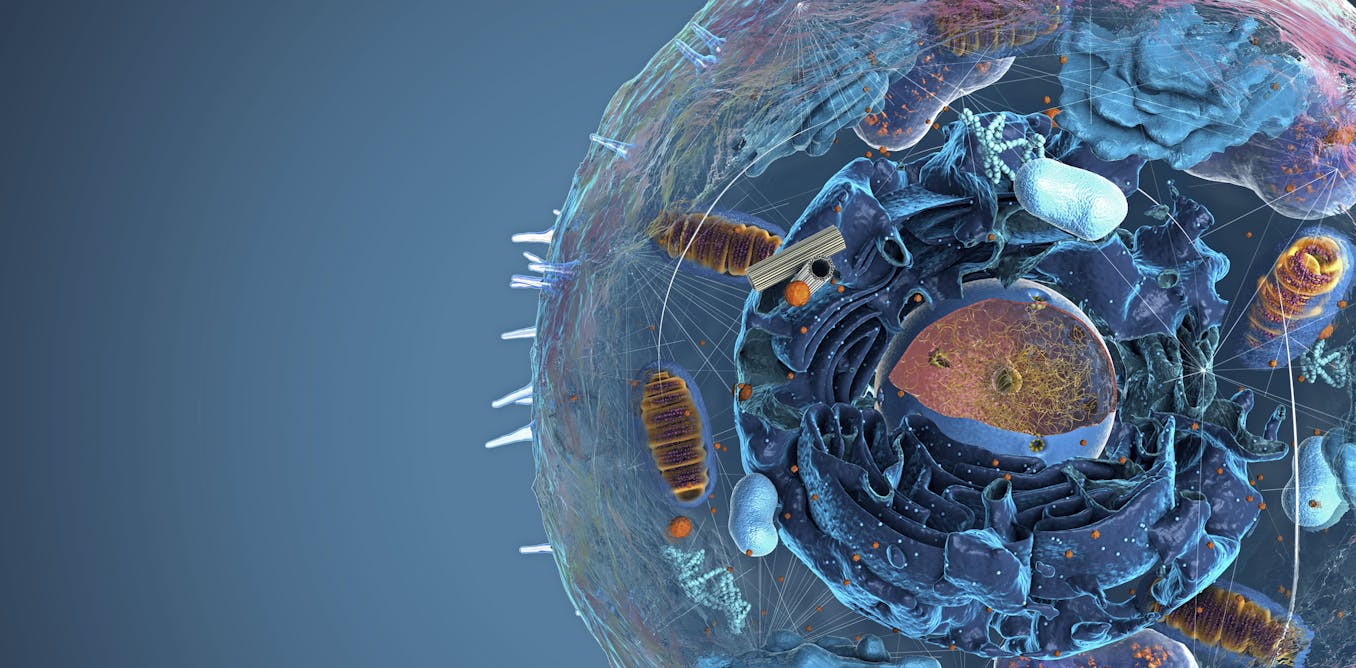
Technology1d agoCells have more mini ‘organs’ than researchers thought − unbound by membranes, these rogue organelles challenge biology’s fundamentals
-

 Technology1d ago
Technology1d agoRussia sends 55 satellites into orbit, including two from Iran | The Express Tribune