Health
'It took the rug right out from under my life': Milestone ME/CFS study begins to explain disease, but will it lead to treatments?
"It took the rug right out from under my life. I went to work that Friday in August; I never went to work a day since, and it'll be 10 years this August."
Those are the words of Jennifer Caldwell, whose life suddenly changed trajectory on an autumn weekend in 2014. Having wrapped up her workweek as a clinical research coordinator the day before, she spent Saturday swimming in her neighborhood pool. But later that day, abdominal pain and violet vomiting episodes sent her to urgent care and then to the ER.
She had colitis, or inflammation of the colon, caused by Clostridioides difficile bacteria, which her doctors treated. However, the infection triggered a debilitating condition that Caldwell lives with to this day: myalgic encephalomyelitis/chronic fatigue syndrome, or ME/CFS. More than 4 million U.S. adults reported having the condition in 2022, but there are not yet any approved treatments for this typically lifelong disease.
Scientists and doctors once thought ME/CFS was a psychological disorder rather than a physical ailment, but over time, data emerged to show that it's in fact a biological illness. Now Caldwell, along with 16 other people with ME/CFS, is helping unravel the biological causes of this understudied condition.
She and the others contributed a trove of data to a landmark National Institutes of Health (NIH) study, published Wednesday (Feb. 21) in the journal Nature Communications, which reveals distinct differences between the bodies of people with ME/CFS and those without it. Differences in brain function and the immune system stand out, in particular, and the data could someday lead to treatments.
Those treatments may not come for a while yet, though, and just this initial study took many years, in part due to disruptions caused by the COVID-19 pandemic.
Related: What ME/CFS can teach us about 'long COVID'
"It was very ambitious to try and throw every test they could think of at a group of patients, and at the time, I thought it was a good idea for a study," said Brian Vastag, one of the study participants, an ME/CFS advocate and a former science reporter for The Washington Post. "But in the end, I just feel so ambivalent about it because it took so long," he told Live Science.
Caldwell, who first contributed data to the study in 2017, told Live Science that she hopes the long-awaited paper helps to validate ME/CFS in the eyes of doctors and the public. "General public has no clue, and 95% of the doctors I've seen … no clue what ME/CFS is," she said.
But both Caldwell and Vastag expressed hope that the study leads to treatments.
"Way back in 2016, when [then-NIH Director] Dr. [Francis] Collins announced this initiative, he did promise the patient community that the study that's being published would just be the first stage," Vastag said. "So they need to follow through, they need to start trials — that would give me some hope."
What the study found
The symptoms of ME/CFS affect many systems in the body and most often set in after an infection caused by bacteria or viruses. The new study focuses on people with this type of post-infectious ME/CFS.
ME/CFS symptoms and their severity can vary among people, but they include losing the ability to engage in physical activity, as well as experiencing thinking problems and sudden dips in blood pressure when changing position. Due to a phenomenon called "post-exertional malaise," the symptoms can suddenly get worse after physical or mental exertion, so people with the condition have to carefully pace themselves to avoid crashing.
Notably, these symptoms often overlap with those of long COVID, a chronic condition that can emerge after a COVID-19 infection and that research suggests frequently shares both clinical and biological features with ME/CFS. Indeed, in the early days of the pandemic, researchers and advocates predicted that the novel coronavirus might trigger the syndrome.
The scientific evidence clearly shows ME/CFS is a disabling, complex and multisystem disease. The medical profession needs to make an effort to learn and understand what patients like me are up against.
Jennifer Caldwell, study participant
Because of this overlap, "whatever we learn from long COVID will be applicable to the ME/CFS and vice versa," senior study author Dr. Avindra Nath, clinical director of the NIH's National Institute of Neurological Disorders and Stroke, told Live Science.
To uncover potential causes of ME/CFS, the NIH recruited 17 people with the syndrome and 21 volunteers without the condition, for comparison. Each person underwent an extensive array of tests, including brain scans, cognitive exams, sleep tests, blood draws, spinal taps and exercise challenges.
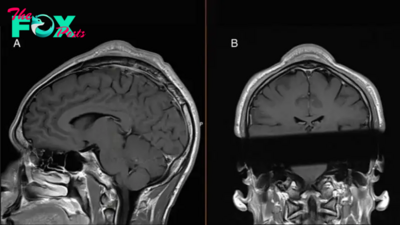
The brain scans measured the flow of oxygenated blood through the brain while participants performed a grip-strength test. These tests revealed that ME/CFS patients showed low activity in a part of the brain called the temporal-parietal junction (TPJ) compared with the comparison group. This brain region checks whether a person is successfully performing an action they're attempting to execute, and it's part of a larger feedback loop that helps control the effort a person exerts and their sense of fatigue.
"It's a functional suppression; it's not a structural damage," Nath said. In other words, the difference seen in the TPJ is a difference in brain activity rather than damage to the brain's physical structure.
Through the spinal taps, the researchers linked ME/CFS to low levels of chemical messengers that are involved in controlling involuntary bodily functions, such as heart rate and blood pressure. These low numbers indicate dysfunction in a hormone-making gland called the hypothalamus, and they also help explain the low TPJ activity. In addition, they hint at why, in people with ME/CFS, the body can't easily adjust its functions to contend with effortful or stressful situations, Nath said.
Related: 'Long flu' is real, and we've likely 'ignored it for a long time'
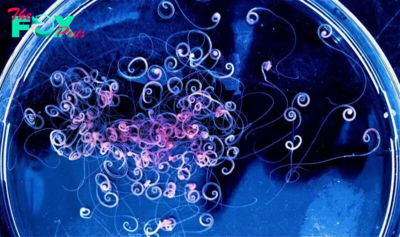
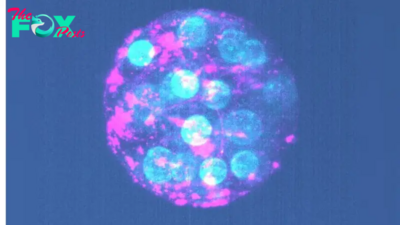
The immune systems of ME/CFS patients also differed from those of the volunteers without the syndrome. For example, they showed signs of T-cell exhaustion, in which immune cells' activity becomes suppressed after they're active for too long. They also carried more naive B cells, immune cells that are broadly reactive and can fight multiple perceived threats to the immune system rather than being trained to attack one foe.
ME/CFS patients' immunity not only differed from that of healthy controls but also differed depending on participants' sex, Nath noted. The study found key distinctions in gene activity, molecular signs of inflammation and immune cell populations between male and female participants. For example, the gene activity of males' T cells appeared disrupted in a way that would affect the cells' ability to activate; meanwhile, female participants carried B cells whose ability to proliferate had been hampered.
"That, I think, is an important part to take forward from this study," Nath said.
What's next?
The results paint a picture of distinct changes in the body and brain and overworked immune systems that drive perpetual inflammation. As Caldwell described it, "It's not good to have your immune jacked up constantly for years. But mine has been, and so your body is constantly battling things that there's no need to be battling." This was previously thought to be a potential cause of ME/CFS, but the new study helps explain what's happening at the level of cells and molecules.
What's more, NIH data published last year suggest that the cells of people with ME/CFS can't easily make new fuel after using it up on a given activity. So the syndrome also may be tied to dysfunction in mitochondria, the powerhouses of cells.
But even with the newly available data, more steps remain before treatments can be developed.
—These 4 risk factors may increase your chance of long COVID, study hints
—Metformin cuts risk of long COVID by 40% in patients with obesity, trial suggests
—Can antiviral drugs prevent long COVID?
"We need to validate these findings, but they can be done in the context of a clinical trial," Nath said. There's now enough data to start pinpointing potential therapies, narrowing down which populations of ME/CFS are likely to benefit, and then testing these in trials. Once selected, multiple drugs could even be tested in the same trial, with, for example, four groups receiving different treatments and one receiving a placebo. This could speed up the process, Nath suggested.
One possible treatment proposed in the study is an existing cancer therapy called immune checkpoint inhibitors. The idea is that ME/CFS patients might have lingering bits of viruses or bacteria that are constantly setting off their immune systems, exhausting their cells. The checkpoint inhibitors could release the brakes of those exhausted T cells, theoretically enabling them to finish the job and clear away the substances continually triggering the immune system.
As these trials get off the ground, ongoing long-COVID treatment trials — including one being led by Nath to test antibodies called IVIG — could also provide hints as to what to try in ME/CFS patients, and vice versa. Vastag argues that the research efforts should be combined, because he says many cases of long COVID are post-infectious ME/CFS.
Although the clinical research is often very slow, he said, scientists need to urgently bring people solutions for ME/CFS.
If you are in crisis, please call, text or chat with the Suicide and Crisis Lifeline at 988, or contact the Crisis Text Line by texting TALK to 741741.
"One thing I want people to know is that this illness is a matter of life and death," he told Live Science. "A lot of patients, they don't have any hope that they will ever get better, and they end up ending their lives." Vastag's life partner, ME/CFS advocate Beth Mazur, died in December 2023 after living with the condition for 15 years, and through the years, Vastag has known others with the disease who died by suicide. It's with that in mind that he hopes the NIH will launch treatment trials expeditiously.
Caldwell, too, hopes trials will start soon. "I would be [the] first one in line because my life — my quality of life is very poor," she said. She spends 90% of her life in bed, leaving the house only to see the doctor or, rarely, to catch one of her daughter's basketball games, she said.
"My biggest reason for wanting to get better is for her," Caldwell said. "There's things for long COVID that they're trying that I would give anything for them to try it for me."
-
 Health13h ago
Health13h agoThe Surprising Benefits of Talking Out Loud to Yourself
-
 Health15h ago
Health15h agoDoctor’s bills often come with sticker shock for patients − but health insurance could be reinvented to provide costs upfront
-

 Health21h ago
Health21h agoHow Colorado is trying to make the High Line Canal a place for everyone — not just the wealthy
-

 Health1d ago
Health1d agoWhat an HPV Diagnosis Really Means
-

 Health1d ago
Health1d agoThere’s an E. Coli Outbreak in Organic Carrots
-
 Health2d ago
Health2d agoCOVID-19’s Surprising Effect on Cancer
-

 Health2d ago
Health2d agoColorado’s pioneering psychedelic program gets final tweaks as state plans to launch next year
-

 Health3d ago
Health3d agoWhat to Know About How Lupus Affects Weight