Health
What do some allergies last a lifetime? Newly described immune cells to blame
Scientists may be a step closer to finally explaining why some allergies can last a lifetime while others fade. Turns out, the persistence of allergies may be linked to a unique type of immune cell.
Allergies have long puzzled scientists — researchers don't fully understand why allergies affect some people but not others, or why allergies emerge in the first place. Previous research has found that the type of antibody most often associated with allergies is produced by cells that don't last very long in the body, which makes people's lifelong allergies harder to explain.
Two new studies, published back-to-back in the journal Science Translational Medicine, might help solve that mystery. The studies, one of which examined children with allergies and the other adults, described a unique type of immune cell that hasn't been tied to allergies before.
Related: The 5 most common seasonal allergies
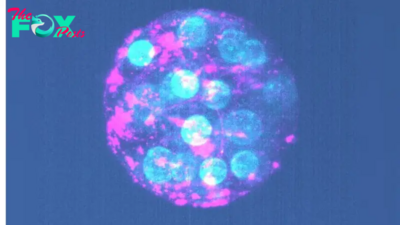
The cells typically produce a type of antibody not associated with allergies, called immunoglobulin G (IgG). But a subset of these cells actually switch over to making an allergy-related antibody called immunoglobulin E (IgE) when confronted with an allergen, whether pollen, pet dander or peanuts.
IgE is usually produced by short-lived plasma cells, which churn out antibodies as an immediate and temporary line of defense for the body. These antibodies are thought to help fight off parasites, for instance, but in allergies, they go after harmless proteins instead.
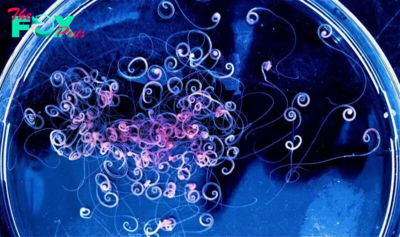
The newly described cells are a type of memory B cell, which typically remember viruses and bacteria and spit out IgG when those invaders show up. But now, scientists have uncovered a subset of memory B cells that remember allergens and can make IgE. These cells are not short-lived like plasma cells and instead linger in the body for an indefinite amount of time — many years, or possibly a person's entire life.
The new research could be helpful in developing new treatments or tests for allergies — for instance, to assess if a childhood allergy is likely to persist into adulthood, the study researchers say.
"These cells may be analyzed as sort of a [biological marker] for risk of allergy or allergy persistence," said Maria Curotto De Lafaille, a professor of pediatrics and of immunology and allergy at the Icahn School of Medicine at Mount Sinai Hospital in New York and senior author of the study on children.
That study focused on children with peanut allergies and analyzed blood samples from 58 kids who are allergic to peanuts and 13 who aren't. The second study analyzed a smaller number of blood samples from adults with a variety of allergies, including six with a birch-pollen allergy, four with a dust-mite allergy and 11 with peanut allergies.
While all the children with allergies avoided eating peanuts, participants in the adult study with birch-pollen allergies gave blood samples before and after starting an immunotherapy treatment for their allergies. This treatment is designed to desensitize the immune system by exposing patients to a small amount of allergen and then gradually increasing the dose over time.
Both studies looked for signs that memory B cells might switch over to producing IgE after being exposed to allergens. For instance, researchers examining samples from children searched for B memory cells with a specific type of receptor, or part of the antibody that enables it to bind to specific proteins. This receptor is more common in people with eczema and asthma, two inflammatory conditions that often coincide with allergies, than in people without the conditions.
Related: Inflammation is a 'mismatch between our evolutionary history and modern environment,' says immunologist Ruslan Medzhitov
The two studies pinpointed the same type of memory B cell in people with allergies, although notably, earlier research had found similar cells in animals and in people with asthma and eczema.
The cells "directly create IgE antibodies, the type that make us allergic," Joshua Koenig, an assistant professor of medicine at McMaster University in Canada and the first author of the paper focused on adults, told Live Science in an email. "They're really the long-term memory reservoir of allergy."
The research is part of "an important area of study, and the key to understanding the persistence of diseases that are caused by antibodies, like allergies," Dr. Sarita Patil, an assistant professor of allergy and immunology at Harvard Medical School who was not involved in the studies, told Live Science in an email.
Both studies were limited by having a small number of participants. Future research could look at how immunotherapy for peanut allergies impacts the newly described cells and the antibodies that they release. It's known that the immunotherapy reduces people's allergen-specific IgE levels over time, but the impact on these memory B cells is unclear.
—What causes metal allergies?
—Can you really be allergic to the sun?
—Allergy vs cold: which is it?
Other future research could see whether the behavior of these cells changes over time, especially in children, who sometimes outgrow their allergies.
Understanding why allergies persist could one day help scientists eliminate or modify these allergy-specific cells so that they don't produce IgE and trigger an immune response anymore, Lafaille said. In other words, studies building on this research might one day help lessen the impact of allergies or even cure them.
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to [email protected] with the subject line "Health Desk Q," and you may see your question answered on the website!
-
 Health1h ago
Health1h agoThe Surprising Benefits of Talking Out Loud to Yourself
-

 Health3h ago
Health3h agoDoctor’s bills often come with sticker shock for patients − but health insurance could be reinvented to provide costs upfront
-

 Health9h ago
Health9h agoHow Colorado is trying to make the High Line Canal a place for everyone — not just the wealthy
-

 Health18h ago
Health18h agoWhat an HPV Diagnosis Really Means
-

 Health1d ago
Health1d agoThere’s an E. Coli Outbreak in Organic Carrots
-

 Health1d ago
Health1d agoCOVID-19’s Surprising Effect on Cancer
-

 Health1d ago
Health1d agoColorado’s pioneering psychedelic program gets final tweaks as state plans to launch next year
-

 Health2d ago
Health2d agoWhat to Know About How Lupus Affects Weight