Health
Pain can linger even after a UTI is gone — haywire nerve growth may explain it
People who experience recurrent urinary tract infections (UTIs) sometimes have lingering pain or still feel the need to pee often, even after their most recent infection has been treated — but now, scientists know why.
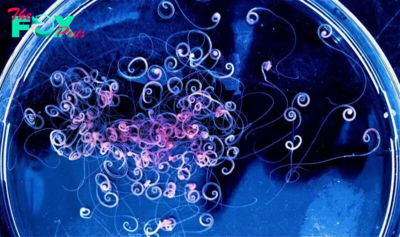
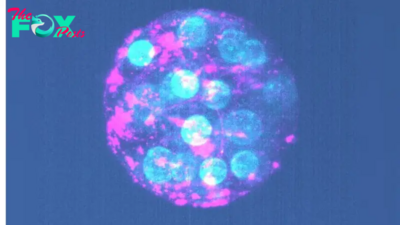
It turns out that bladder damage caused by recurrent infections can drive immune cells called mast cells to release chemicals that drive the overgrowth of nearby nerves. These nerves are then more likely to transmit signals to the brain that are interpreted as either pain or the sensation that the bladder is full, even if it's not. The mast cells also spew inflammatory molecules called histamines that further rev up pain receptors in these nerves, even in the absence of an active infection.
The new findings, published Friday (March 1) in the journal Science Immunology, come from a small study conducted using tissue samples from human patients' bladders and more detailed analyses in mice. Although it's still early days, the research suggests that it may be important to develop treatments that target nerve outgrowth in these patients, the authors say. Such therapies could be used as an add-on to the initial antibiotics used to treat a person's infection.
Related: Bacteria from meat may cause a half-million UTIs a year
An explosion of nerve growth
UTIs are bacterial infections of the urinary system, which includes the bladder, kidneys, and the tubes that run between these structures and to the outside of the body. Common symptoms include the feeling of needing to pee more often than usual and experiencing pain while doing so.
Around 80% of all UTI cases occur in women. Many develop recurrent UTIs, defined as having two "episodes" of infection and associated symptoms within six months of each other. UTIs are usually cleared within days of someone starting antibiotics, but sometimes their symptoms can persist.
To investigate why, Abraham and colleagues analyzed tissue samples taken from the bladders of eight women who experienced recurrent UTIs and three who didn't. The patients in the former group were experiencing symptoms of a UTI at the time of the study but did not have bacteria in their urine, suggesting they didn't have active infections.
The researchers found that the tissues from people with recurrent UTIs contained a much higher number of nerves. Separately, when they compared urine samples from 25 women who experienced recurrent UTIs to those from 12 women with no history of the infections, they found that the former group had higher concentrations of a protein called Substance P, which nerves make when activated.
To see if these differences appear due to recurrent UTIs, the team experimented with mice. They infected the mice once a week with UTI-causing microbes, for three consecutive weeks. Compared to mice who hadn't been infected, the mice with recurrent UTIs needed to pee more often and were more sensitive to being touched around the pelvis.
A close look at the rodents' bladders revealed that they shared many of the same characteristics seen in the human tissue samples.
Related: Fatal 'brain-eating' amoeba successfully treated with repurposed UTI drug

"We saw the nerves had sprouted all over — they had increased in length and had many more branch points," Soman Abraham, co-senior study author and a professor of pathology at the Duke University School of Medicine in North Carolina, told Live Science. They also saw that mast cells located near the nerves were producing a growth chemical called nerve growth factor (NGF).
When you have a UTI, the bladder sheds its outer lining to help rid itself of the bacteria causing the infection, Abraham said. However, nearby nerve cells are also shed in this process, which the body then tries to replace. In people with recurrent UTIs, this system seems to kick into overdrive and ultimately spur too much nerve growth.
In another experiment, the team blocked NGF production in mice with recurrent UTIs; this prevented the nerve overgrowth and reduced symptoms of the disease.
—How much urine can a Healthy bladder hold?
—What turned this woman's pee a striking shade of lilac?
—Finally, we know why pee is yellow
These findings need to be confirmed in further studies, including in experiments with larger animals, before they could be used to develop any kind of treatment that could be tested in humans. However, these initial observations suggest that developing therapies to prevent nerve outgrowth could offer "better and earlier relief" from the "most pressing symptoms" experienced by people with recurrent UTIs, the authors wrote in the paper.
In theory, such treatments could also help cut back on the doctors prescribing antibiotics when they're not needed. If a patient doesn't have an active UTI, antibiotics won't help diminish their symptoms, but perhaps an alternative treatment could. The overuse of antibiotics can both have knock-on effects in patients — disrupting their gut microbiomes, for example — and contribute to the rise of antibiotic resistance.
This article is for informational purposes only and is not meant to offer medical advice.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun? Send us your questions about how the human body works to [email protected] with the subject line "Health Desk Q," and you may see your question answered on the website!
-

 Health16h ago
Health16h agoTeens Are Stuck on Their Screens. Here’s How to Protect Them
-

 Health21h ago
Health21h agoHow Pulmonary Rehab Can Help Improve Asthma Symptoms
-
 Health21h ago
Health21h ago10 Things to Say When Someone Asks Why You’re Still Single
-
 Health2d ago
Health2d agoThe Surprising Benefits of Talking Out Loud to Yourself
-

 Health2d ago
Health2d agoDoctor’s bills often come with sticker shock for patients − but health insurance could be reinvented to provide costs upfront
-

 Health2d ago
Health2d agoHow Colorado is trying to make the High Line Canal a place for everyone — not just the wealthy
-

 Health2d ago
Health2d agoWhat an HPV Diagnosis Really Means
-

 Health2d ago
Health2d agoThere’s an E. Coli Outbreak in Organic Carrots